 People with interstitial lung disease usually come to see a doctor due to concern about shortness of breath or cough that has progressed over time. Usually patients will not develop symptoms until the disease has progressed. Some will have an acute presentation or episode of worsening, also called acute exacerbation.
People with interstitial lung disease usually come to see a doctor due to concern about shortness of breath or cough that has progressed over time. Usually patients will not develop symptoms until the disease has progressed. Some will have an acute presentation or episode of worsening, also called acute exacerbation.
History & Physical Exam: Diagnosis of ILDs begins with a detailed medical history focusing on co morbidities, medication use, environmental exposures and family history, followed by a thorough physical examination. The physician may hear crackles or Velcro-like sounds using the stethoscope.
 Chest X-ray: A routine chest X-ray is the first test in the evaluation of most people. Chest X-ray films in people with ILD may show fine scarring of the lungs. However, ILD cannot be diagnosed using a chest X-ray alone.
Chest X-ray: A routine chest X-ray is the first test in the evaluation of most people. Chest X-ray films in people with ILD may show fine scarring of the lungs. However, ILD cannot be diagnosed using a chest X-ray alone.
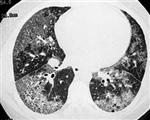 High-Resolution CT Scan: If ILD is suspected, a detailed image of the lungs in the form of HRCT may show specific radiologic patterns to indicate different types of the disease. A radiologist may identify ‘honeycombing’ to indicate scarring of the lung or ‘ground glass haze’ to suggest inflammation of the lung tissue. In the commonest form of ILDs known as Idiopathic Pulmonary Fibrosis ( IPF)
High-Resolution CT Scan: If ILD is suspected, a detailed image of the lungs in the form of HRCT may show specific radiologic patterns to indicate different types of the disease. A radiologist may identify ‘honeycombing’ to indicate scarring of the lung or ‘ground glass haze’ to suggest inflammation of the lung tissue. In the commonest form of ILDs known as Idiopathic Pulmonary Fibrosis ( IPF)
 Pulmonary Function Testing: A person is made to breathe through a tube connected to a computerzed spirometer machine that measures the total amount of air within the lungs. People with ILD may have a reduced total lung capacity. In addition, they may also have a decreased lung to blood oxygen-transfer ability.
Pulmonary Function Testing: A person is made to breathe through a tube connected to a computerzed spirometer machine that measures the total amount of air within the lungs. People with ILD may have a reduced total lung capacity. In addition, they may also have a decreased lung to blood oxygen-transfer ability.
Pulse Oximeter Readings: 6 Minutes Walk Test & Arterial Blood Gas (ABG): A device is placed on the finger or earlobe to signify the oxygenation in the blood. Normal ranges are 95-100% on room air. The patient may be asked to walk for a certain time in his own stride so that the distance walked in that time and the desaturation of oxygen in his blood is measured. ABG is done to further indicate how much oxygen is actually available to the body and also measures carbon dioxide levels.
Broncho Alveolar Lavage (BAL): Using a bronchoscope, a sample of cells from the lower respiratory tract is collected by instilling a small amount of saline. This may often guide the pulmonologist in the diagnosis of various ILDs.
Video-Assisted Thoracoscopic Surgery (VATS): VATS is a minimally invasive procedure to sample multiple areas of lung tissue for histopathology. It may be needed to confirm some conditions or when the diagnosis is unclear by clinical and radiological information.
 The clinical course of the disease may vary according to the type of ILD and its cause. The options available to manage patients and maintain their quality of life are broadly divided into pharmacological and non pharmacological treatment options.
The clinical course of the disease may vary according to the type of ILD and its cause. The options available to manage patients and maintain their quality of life are broadly divided into pharmacological and non pharmacological treatment options.
PHARMACOLOGICAL:
Corticosteroids: Normally, the adrenal glands produce a hormone called cortisol. Corticosteroids such as prednisone and methylprednisolone that are used in the treatment of ILDs mimic the action of this hormone. The purpose is to reduce the inflammation in the body by suppressing the immune system. Because of the same reason, a person may become prone to developing infections more often. Hence, patients receiving prolonged treatment or high dose steroids will require careful monitoring.
N-Acetyl Cysteine (NAC): This potent antioxidant is still under study. It may slow the decline of lung function in some forms of ILD. It should not be used alone.
Azathioprine and Methotrexate: These are also immune system suppressants which are sometimes used in certain types where studies suggest they might help in ILD.
The Anti Fibrotic Drugs:
Pirfenidone (PIRFENEX, ESBRIET): Pirfenidone was approved by FDA (2014) as an anti fibrotic drug for the treatment of patients with mild to moderate IPF. It had been available in the EU, Canada and some parts of Asia even before this. Common side effects include gastrointestinal discomfort and photosensitivity rash. It is still not a registered drug in Pakistan and hence it availability remains a problem.
Nintedanib (OFEV): Nintedanib is another anti-fibrotic drug that has been shown to slow down the decline in lung functions in IPF patients. Common side effects include abdominal pain, vomiting and diarrhea. This drug is not available in Pakistan.
NON PHARMACOLOGICAL:
Oxygen Therapy: In patients with low oxygen blood levels (detected by pulse oximetry or ABG) due to ILD, inhaled oxygen may improve symptoms. Regular use of oxygen might also protect the heart from damage caused by low oxygen levels.
Pulmonary Rehabilitation: It includes conditioning; exercise training and breathing exercises; anxiety, stress, and depression management; nutritional counseling; education; and other components. The goal of pulmonary rehabilitation is to restore the patient’s ability to function without extreme breathlessness, therefore should be offered to patients with stable IPF. PR can improve the walking distance and quality of life. The patients with advanced disease may not be suitable candidates for PR.
Using a multidisciplinary approach, palliative care can involve physical, psychosocial, and spiritual factors as a part of management plan.
Lung transplant : In advanced stage ILD causing severe impairment, a lung transplant may be the advised option. However, this is not yet available in our geographical vicinity
- + Symptoms
-
 People with interstitial lung disease usually come to see a doctor due to concern about shortness of breath or cough that has progressed over time. Usually patients will not develop symptoms until the disease has progressed. Some will have an acute presentation or episode of worsening, also called acute exacerbation.
People with interstitial lung disease usually come to see a doctor due to concern about shortness of breath or cough that has progressed over time. Usually patients will not develop symptoms until the disease has progressed. Some will have an acute presentation or episode of worsening, also called acute exacerbation. - + Diagnosis of ILDs
-
History & Physical Exam: Diagnosis of ILDs begins with a detailed medical history focusing on co morbidities, medication use, environmental exposures and family history, followed by a thorough physical examination. The physician may hear crackles or Velcro-like sounds using the stethoscope.
 Chest X-ray: A routine chest X-ray is the first test in the evaluation of most people. Chest X-ray films in people with ILD may show fine scarring of the lungs. However, ILD cannot be diagnosed using a chest X-ray alone.
Chest X-ray: A routine chest X-ray is the first test in the evaluation of most people. Chest X-ray films in people with ILD may show fine scarring of the lungs. However, ILD cannot be diagnosed using a chest X-ray alone. High-Resolution CT Scan: If ILD is suspected, a detailed image of the lungs in the form of HRCT may show specific radiologic patterns to indicate different types of the disease. A radiologist may identify ‘honeycombing’ to indicate scarring of the lung or ‘ground glass haze’ to suggest inflammation of the lung tissue. In the commonest form of ILDs known as Idiopathic Pulmonary Fibrosis ( IPF)
High-Resolution CT Scan: If ILD is suspected, a detailed image of the lungs in the form of HRCT may show specific radiologic patterns to indicate different types of the disease. A radiologist may identify ‘honeycombing’ to indicate scarring of the lung or ‘ground glass haze’ to suggest inflammation of the lung tissue. In the commonest form of ILDs known as Idiopathic Pulmonary Fibrosis ( IPF) Pulmonary Function Testing: A person is made to breathe through a tube connected to a computerzed spirometer machine that measures the total amount of air within the lungs. People with ILD may have a reduced total lung capacity. In addition, they may also have a decreased lung to blood oxygen-transfer ability.
Pulmonary Function Testing: A person is made to breathe through a tube connected to a computerzed spirometer machine that measures the total amount of air within the lungs. People with ILD may have a reduced total lung capacity. In addition, they may also have a decreased lung to blood oxygen-transfer ability.Pulse Oximeter Readings: 6 Minutes Walk Test & Arterial Blood Gas (ABG): A device is placed on the finger or earlobe to signify the oxygenation in the blood. Normal ranges are 95-100% on room air. The patient may be asked to walk for a certain time in his own stride so that the distance walked in that time and the desaturation of oxygen in his blood is measured. ABG is done to further indicate how much oxygen is actually available to the body and also measures carbon dioxide levels.
Broncho Alveolar Lavage (BAL): Using a bronchoscope, a sample of cells from the lower respiratory tract is collected by instilling a small amount of saline. This may often guide the pulmonologist in the diagnosis of various ILDs.
Video-Assisted Thoracoscopic Surgery (VATS): VATS is a minimally invasive procedure to sample multiple areas of lung tissue for histopathology. It may be needed to confirm some conditions or when the diagnosis is unclear by clinical and radiological information.
Surgical Lung Biopsy (Thoracotomy): Traditional surgery of the chest is needed in some cases to obtain a lung biopsy. - + Treatment
-
 The clinical course of the disease may vary according to the type of ILD and its cause. The options available to manage patients and maintain their quality of life are broadly divided into pharmacological and non pharmacological treatment options.
The clinical course of the disease may vary according to the type of ILD and its cause. The options available to manage patients and maintain their quality of life are broadly divided into pharmacological and non pharmacological treatment options.PHARMACOLOGICAL:
Corticosteroids: Normally, the adrenal glands produce a hormone called cortisol. Corticosteroids such as prednisone and methylprednisolone that are used in the treatment of ILDs mimic the action of this hormone. The purpose is to reduce the inflammation in the body by suppressing the immune system. Because of the same reason, a person may become prone to developing infections more often. Hence, patients receiving prolonged treatment or high dose steroids will require careful monitoring.
N-Acetyl Cysteine (NAC): This potent antioxidant is still under study. It may slow the decline of lung function in some forms of ILD. It should not be used alone.
Azathioprine and Methotrexate: These are also immune system suppressants which are sometimes used in certain types where studies suggest they might help in ILD.
The Anti Fibrotic Drugs:
Pirfenidone (PIRFENEX, ESBRIET): Pirfenidone was approved by FDA (2014) as an anti fibrotic drug for the treatment of patients with mild to moderate IPF. It had been available in the EU, Canada and some parts of Asia even before this. Common side effects include gastrointestinal discomfort and photosensitivity rash. It is still not a registered drug in Pakistan and hence it availability remains a problem.
Nintedanib (OFEV): Nintedanib is another anti-fibrotic drug that has been shown to slow down the decline in lung functions in IPF patients. Common side effects include abdominal pain, vomiting and diarrhea. This drug is not available in Pakistan.NON PHARMACOLOGICAL:
Oxygen Therapy: In patients with low oxygen blood levels (detected by pulse oximetry or ABG) due to ILD, inhaled oxygen may improve symptoms. Regular use of oxygen might also protect the heart from damage caused by low oxygen levels.
Pulmonary Rehabilitation: It includes conditioning; exercise training and breathing exercises; anxiety, stress, and depression management; nutritional counseling; education; and other components. The goal of pulmonary rehabilitation is to restore the patient’s ability to function without extreme breathlessness, therefore should be offered to patients with stable IPF. PR can improve the walking distance and quality of life. The patients with advanced disease may not be suitable candidates for PR.
Using a multidisciplinary approach, palliative care can involve physical, psychosocial, and spiritual factors as a part of management plan.
Lung transplant : In advanced stage ILD causing severe impairment, a lung transplant may be the advised option. However, this is not yet available in our geographical vicinity
- + Spiritual Support
-
Update Required To play the media you will need to either update your browser to a recent version or update your Flash plugin.







