 Interstitial Lung Disease (ILD) is a heterogeneous group of non-infectious, non-malignant diffuse parenchymal disorders of the lower respiratory tract, affecting the alveolar wall structure and often small airways and blood vessels of the lung parenchyma. The most important of these is the idiopathic pulmonary fibrosis.
Interstitial Lung Disease (ILD) is a heterogeneous group of non-infectious, non-malignant diffuse parenchymal disorders of the lower respiratory tract, affecting the alveolar wall structure and often small airways and blood vessels of the lung parenchyma. The most important of these is the idiopathic pulmonary fibrosis.
There are more than 300 different types of ILDs present. For practical purposes, they are broadly classified into either those with an identifiable cause or idiopathic i.e. without a known etiology. Known causes include genetics/hereditary, drug-induced, collagen vascular related, hypersensitivity pneumonitis and occupational exposures such as asbestos and silica. Etiology in a majority of cases remains unidentified and such ILD types include idiopathic pulmonary fibrosis, non-specific interstitial pneumonias, sarcoidosis, respiratory bronchiolitis ILD and so on.
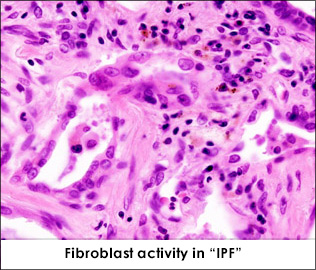
Usual specific symptoms include difficulty in breathing, especially on exertion and persistent dry cough, but these may vary. In addition, systemic signs and auscultatory findings help to guide clinically towards the diagnosis of ILD. Diagnostic investigations include imaging studies such as chest x-ray and high resolution computed tomography (HRCT) of the chest. Each type of ILD manifests a different pattern on the HRCT. Pulmonary function tests (PFTs) typically show a restrictive pattern and a ventilatory defect. However, confirmation of diagnosis warrants a biopsy of the lung tissue. Ideally, the diagnosis of ILD should be based on a multidisciplinary approach involving a pulmonologist, radiologist and histopathologist.
Current therapy includes new anti-fibrotic agents aimed at slowing the progression of the disease. Many clinical trials are underway, raising hope of having better treatment options in the future for patients with ILD.

